Problem?
Michael E. Ash BSc (Hons) DO. ND. F.Dip ION reviews the latest studies on this pathogen.
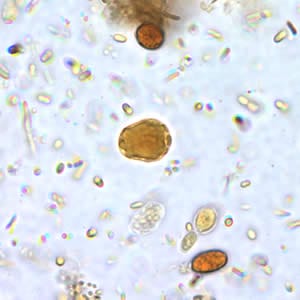
Blastocystis is an unusual enteric protozoan parasite of humans and many animals. It has a worldwide distribution and is often the most commonly isolated organism in parasitological surveys. The parasite has been described since the early 1900s, but only in the last decade or so have there been significant advances in the understanding of Blastocystis biology.
Despite years of study, the pathogenic role of Blastocytis hominis is still regarded by some as controversial. It is thought that establishing relevant genotypic differences between the asymptomatic and symptomatic isolates should assist in determining the pathogenicity of Blastocystis by clearly assigning symptoms to genotype.
In a recent study, the researcher’s genotyped 32 Blastocystis isolates obtained from 12 asymptomatic healthy individuals and 20 symptomatic patients. They used polymerase chain reaction techniques to identify the known seven kinds of sequence tagged subtype primers. When they compared genotype of Blastocystis isolates between the symptomatic and asymptomatic patient group, they found that subtype 3 is the most dominant genotype in asymptomatic individual (9/12) and subtype 1 determined all of symptomatic patients (20/20).[1] Suggesting that variations in the genetic makeup can have significant impact on the likelihood of an individual experiencing symptoms.
Comment
This genetic investigation is not undertaken by standard pathology labs. If it was more readily available, B.hominis spp subtypes, known to be of ‘nil’ pathogenicity could be either ignored or treated prospectively. Patients who in the past have been treated and shown benefit on elimination of B.hominis most likely were infected with the species that met the genetic requirements for pathogenic response, and those treated but post eradication had no improvement may have had other confounding pathogens or underlying health problems.
New Insights on Classification, Identification, and Clinical Relevance of Blastocystis spp
Further clarification of this ubiquitous organism can be found in the excellent free review by Kevin Tan: Clinical Microbiology Reviews; published in Oct. 2008.[2]
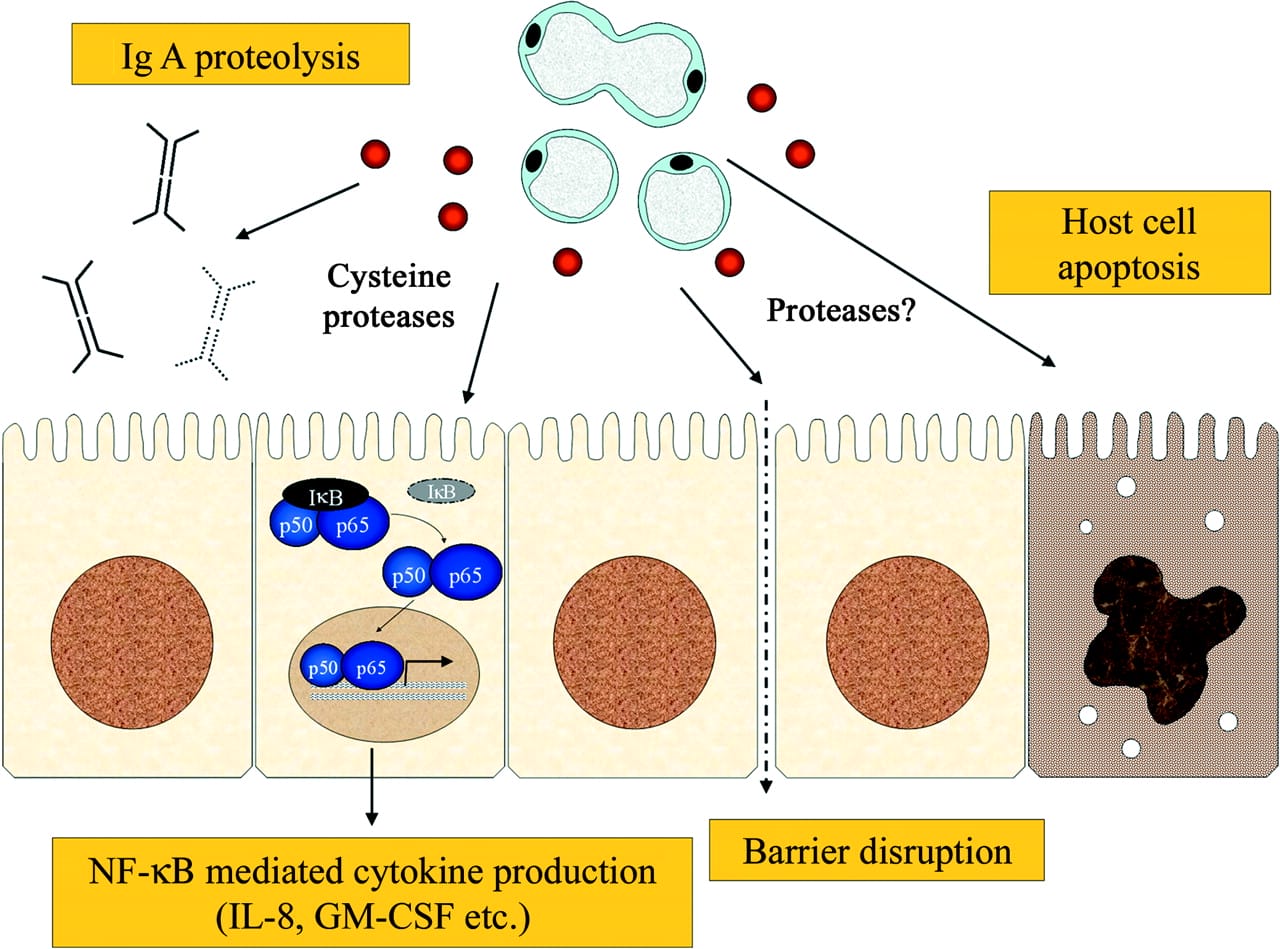
The image below is extracted from the article and simplifies a model for pathogenesis of Blastocystis spp. It shows how Blastocystis infection may result in a variety of pathological outcomes such as secretory IgA degradation, barrier function compromise, host cell apoptosis, and induction of proinflammatory cytokines.
SIgA degradation and barrier disruption may promote the growth and invasion of local gastrointestinal pathogens or the expansion of commensal organisms, that by virtue of their different ratio become problematic. This can explain the apparent dysbiosis found in patients with B.hominis confirmed. The degradation of SIgA also contributes to loss of bacterial balance and will reduce the competence of regulatory T Cells (Treg) production which in turn may increase the risk of proinflammatory related para-inflammation local to the gut and systemically.
Pathogenicity
Clinical features of illness that have been attributed to Blastocystis spp. are nonspecific and include nausea, anorexia, abdominal pain, bloating, flatulence, and acute or chronic diarrhoea. Of these features, the most commonly recorded symptoms among patients are abdominal pain and diarrhoea.[3] Symptoms can be variable, ranging from mild diarrheal illness[4] and chronic diarrhoea[5] to acute gastroenteritis.[6]
One study has described an association between infection density and allergic cutaneous diseases. In a study of Blastocystis-positive patients from a Turkish hospital, the criteria for selection were the absence of any other co-infecting pathogens and the presence of more than five parasites per high-power field. The symptoms from this group were abdominal pain (76.9%), diarrhoea (50%), distension (32.6%), and urticaria (5.7%), suggesting an association between parasite density and pathology.[7] Other signs and symptoms associated with Blastocystis infections include faecal leukocytes, eosinophilia, and cutaneous rashes, particularly urticaria.[8],[9],[10]
Accumulating reports also suggest an association between Blastocystis and irritable bowel syndrome (IBS), a functional bowel disorder in which abdominal pain is associated with a defect or a change in bowel habits.[11] In two studies[12],[13]Blastocystis was detected more frequently in IBS patients than in a control group consisting of IBS-negative patients with gastrointestinal symptoms.
Eradication
This is a more controversial area, as the use of Metronizadole (Flagyl) is often the first recommended intervention but can be ineffective. The cyst form has been shown to be resistant (up to 5 mg/ml) to the cytotoxic effect of the drug.
Those observations, together with the extensive genetic heterogeneity of the organism, may offer explanations for the variability in drug susceptibilities and treatment failures. A summary list of drug interventions may be found in the Tan article.
Studies to investigate the usefulness of cotrimoxazole in Blastocystis infections and Nitazoxanide, a 5-nitrothiazole broad-spectrum antiparasitic agent, have been reported to be effective against Blastocystis.
Paromomycin, a broad-spectrum antibiotic indicated for acute and chronic intestinal amoebiasis, was shown to successfully treat Blastocystis infections associated with cutaneous lesions, predominantly urticaria.
Iodoquinol has been suggested to be a suitable eradicator of this organsim. Metronidazole, iodoquinol, or co-trimoxazole has been reported to be effective in Blastocystis infections, but metronidazole resistance may be common.
Natural Strategies
- Establish support for SIgA production using Saccharomyces Boulardii, also prescribe with any antibiotic therapy to reduce loss of commensals. SB also inhibits IL-8 and reduces inflammation
- Introduce a natural antimicrobial, this can include, standardised oil of oregano, black walnut, artemesinin, berberine sulphate, citrus seed extract.
- Restoring the microbial ecology with the use of suitable probiotics and immune supporting nutrients especially Vit A for the modification of Treg activity and glutamine for barrier integrity.
Treatment may not be required if the B.hominis is not of the pathogenic type, other agents may be causing the symptoms. The use of medications may be judged by the severity of the symptoms and prior use. The long term success of eradication will depend on the successful restoration of mucosal immune function and the continued non exposure to repeat infection.
References
[1] Eroglu F, Genc A, Elgun G, & Koltas IS (2009). Identification of Blastocystis hominis isolates from asymptomatic and symptomatic patients by PCR. Parasitology research, 105 (6), 1589-92 PMID: 19685075
[2] Tan, K. (2008). New Insights on Classification, Identification, and Clinical Relevance of Blastocystis spp. Clinical Microbiology Reviews, 21 (4), 639-665 DOI: 10.1128/CMR.00022-08
[3] El-Shazly, A. M., A. A. Abdel-Magied, S. N. El-Beshbishi, H. A. El-Nahas, M. A. Fouad, and M. S. Monib. 2005. Blastocystis hominis among symptomatic and asymptomatic individuals in Talkha Center, Dakahlia Governorate, Egypt. J. Egypt. Soc. Parasitol. 35:653-666. View Abstract
[4] Rossignol, J. F., S. M. Kabil, M. Said, H. Samir, and A. M. Younis. 2005. Effect of nitazoxanide in persistent diarrhea and enteritis associated with Blastocystis hominis. Clin. Gastroenterol. Hepatol. 3:987-991 View Abstract
[5] Rossignol, J. F., S. M. Kabil, M. Said, H. Samir, and A. M. Younis. 2005. Effect of nitazoxanide in persistent diarrhea and enteritis associated with Blastocystis hominis. Clin. Gastroenterol. Hepatol. 3:987-991 View Abstract
[6] Andiran, N., Z. C. Acikgoz, S. Turkay, and F. Andiran. 2006. Blastocystis hominis—an emerging and imitating cause of acute abdomen in children. J. Pediatr. Surg. 41:1489-1491. View Abstract
[7] Kaya, S., E. S. Cetin, B. C. Aridogan, S. Arikan, and M. Demirci. 2007. Pathogenicity of Blastocystis hominis, a clinical reevaluation. Turkiye Parazitol. Derg. 31:184-187. View Abstract
[8] Diaczok, B. J., and J. Rival. 1987. Diarrhea due to Blastocystis hominis: an old organism revisited. South. Med. J. 80:931-932. View Abstract
[9] Garavelli, P. L. 1991. The therapy of blastocystosis. J. Chemother. 3(Suppl. 1):245-246. View Abstract
[10] Armentia, A., J. Mendez, A. Gomez, E. Sanchis, A. Fernandez, R. de la Fuente, and P. Sanchez. 1993. Urticaria by Blastocystis hominis. Successful treatment with paromomycin. Allergol. Immunopathol. (Madrid) 21:149-151
[11] Giacometti, A., O. Cirioni, A. Fiorentini, M. Fortuna, and G. Scalise. 1999. Irritable bowel syndrome in patients with Blastocystis hominis infection. Eur. J. Clin. Microbiol. Infect. Dis. 18:436-439. View Abstract
[12] Giacometti, A., O. Cirioni, A. Fiorentini, M. Fortuna, and G. Scalise. 1999. Irritable bowel syndrome in patients with Blastocystis hominis infection. Eur. J. Clin. Microbiol. Infect. Dis. 18:436-439. View Abstract
[13] Govind, S. K., A. A. Khairul, and H. V. Smith. 2002. Multiple reproductive processes in Blastocystis. Trends Parasitol. 18:528. View Abstract






121 Comments. Leave new
I completely agree with you, Michael. The range of symptoms presenting in individuals harbouring Blastocystis is staggering.
Having worked with many people with H pylori, I’d also like to add that Blasto infection is often concomitant with H pylori (like a double act).
I personally had Blasto and H pylori, successfully clearing them using herbal protocols and IgA/mucosal restoration.
Keep up the good work!
Dave Hompes
Dear Dave
Thank you for your feedback, you are correct in that there are frequently co infections as B.hominis is only able to survive in a mucosally (immune) compromised host. I will be reviewing other pathogens over the coming weeks and hope to explain the relationships such as the one you describe with B.hominis and H.pylori.
Fascinating to see the subtype 1 finding from Eroglu et al. Reference a 6 year old with symptomatic blastocystis hominis, what would the natural protocol be? I understand that glutamine is not recommended for this agegroup.
Dear Catharine
The resolution of B.hominis must also include a programme of immune support for all patients as B.h degrades SIgA and with this protein diminished barrier function will decline. A 6 year old will not have reached maturity of SIgA production anyway. This is achieved at age 7.
The use of herbal standardised extracts must also be undertaked cautiously with all patients, espescially children. The Oil of oregano (ADP – 100mg), SB(250-50mg) and LGG (1 cap) at a dose indicated in brackets may be used as a guide line. The duration will depend on the resilience of the species and tolerance to intervention but expect at least 6-8 weeks of treatment and then re-test. Look for confounding issues such as dimished bacterial populations and other pathogens. If the Oil is rejected because of the taste consider pure artemisinin or Qinghaosu, the active constituent of the herb Artemisia annua (sweet wormwood) at 200mg in two divided doses of 100mg each.
Michael
I read the article above and it was somewhat useful. I am going to give it to my daughters doctor. My 16 year old returned after spending a month in Turkey with this parasite. Do these parasites lay their eggs in the liver and if they do how does one eradicate them from maturing. At the moment my daughter is on the antibiotic mentioned above. the treatment seems to be worse than the parasite itself.She is losing body mass and goes in and out of vertigo and nausea. The doctor has said that this is normal.Is this true? I am at my wits end in treating this condition. Any suggestions? Do you know of any specialists in new york city whom I could take her to? Feeding her has been so problematic, do you have any suggestions as to diet?
Thanking you in advance for attending to my inquories.
Worried Mom
Dear Elvira
I am unable to give personal advice, I can however, offer some overall information you may find helpful.
B.hominis matures and reproduces in the intestinal tract of humans and animals. It is unclear as to which mechanism is most frequently employed for population expansion – but this is under investigation. Upon ingestion of cysts, the parasite undergoes excystation (The release of the internal (ie, encysted) contents (eg, trophozoites or sporozoites) from cysts or oocysts) in the large intestines and develops into vacuolar forms. Encystation (the process of forming a cyst or becoming enclosed in a capsule) occurs during passage along the large intestines and is deposited in the faeces. In simple terms the cysts infect epithelial cells of the digestive tract and multiply asexually.
Do extraintestinal infections with Blastocystis spp. occur, such as in the liver? There seems to be no absolute negative to this question, but appears that if there was liver infiltration it would most likely be mediated by some other pathogen.
Adverse reactions to medications are common. You do not define which medicine you have been presribed, the article mentioned the most commonly used but there are many.
Natural agents as well as dietary recommendations are best discussed with a suitably qualified clinician. Dr Leo Galland may be considered, or search for functional medicine clinicians in the New York area by visiting this web site or rediscuss with your own Dr. As a rule of thumb treatment should not be worse than the infection!
Michael
Hi, I am doing a lot of personal research relating to my recently diagnosed high level of blastocystis hominis, citrobacter freundi (4+), klebsiella pneuoniae (4 +), evidence of a slightly low level of stomach acid and lowered level of bowel flora (missing Lactobacillus species). I appreciate that you are limited on the advice that can be given, but the research I have done so far suggests that parasites feed on bacteria – friendly or otherwise – so my use of probiotics may be feeding the parasite. I obviously need to get my Lactobacillus levels up but should I aim to eradicate the parasite first before I tackle this? And can I tackle the citrobacter and klebsiella at the same time as the parasite? I’m also keen to go down the nutrional path to fight these and should be grateful if someone could point me in the direction of some advice relating to this. Incidently, I ended up having the tests that showed up the above results as a consequence of developing a body odour that ranges from foul (smelling of faeces) to unpleasant. Strangly, only children and a tiny number of adults smell this odour but being a teacher, it has stopped me teaching over the last six months as I could no longer tolerate the cruel comments of children. As my GP could not smell the odour, I was treated as though the problem was in my mind – have you ever come across others with this odour problem? (NB the odour was not coming from armpits etc and personal hygiene is secong to none!). Hoping that you are able to pass on some thoughts.
Hi Rosemary.
The starting point for your current GI status is to see that there is a loss of bacterial control over the intestinal habitat. This may be created by a variety of factors, one contributor is the shortfall in HCL, an essential part of the chemical mix that perpetuates the internal bacterial colonisation by commensals.
B. hominis is a parasite, a microscopic single-celled organism (protozoan). It behaves like a tiny animal — hunting and gathering other microbes for food and this will include bacteria found in its environment as well as other matter.
This is part of the normal life-cycle of all protozoans and should not be confused with the idea that delivering quantities of beneficial bacteria will create axtra food. The doses you can deliver will never match the voluminous amounts of bacteria already present. There has been a question about the long term use of antibiotics as a therapeutic adjunct, but I would suggest this does not make good clinical sense.
So it is sensible to address the bacterial imbalance by using suitable lactic acid bacteria, here you will be populating the small intestine and the the species L.Rhamnosus (LGG) and Plantarum, Salivarius (LRPS) are species that distribute their activities from the proximal to the distal part of the small intestine. It is also sensible to consider the health of your gall bladder as bile acids are an important component of bacterial balance and mucosal immunity. I have written on this here.
It is practical to separate anti microbial therapy, whether drug based or not from the delivery of probiotics by a few hours at least. Take the probiotics with food also. General antimicrobials such as olive leaf extract, black walnut hulls, citrus seed extract and oregano will produce changes in all pathogens described at differing combination’s and dose.
Body odour with selective recognition is certainly an unusual symptom and may reflect a type of selective hyposmia (a decreased ability to smell) by those unable to smell it, or a selective increased sensitivity by those, including yourself who could, this is called hyperosmia. Aside from the complications of this life changing odour, the question is, can parasites or the conditions that permit parasites to exist cause changes in body odour? It is worth remembering that B.hominis is pathogenic or is an opportunistic pathogen, with immunocompromised populations being more susceptible to infection and its associated symptoms and it may be another organism as yet unidentified that has caused this change.
The answer is: yes parasites and or dysbiosis can cause a change in body odour. Infection and body odours: Evolutionary and medical perspectives
Infection, Genetics and Evolution, Volume 9, Issue 5, September 2009, Pages 1006-1009 Franck Prugnolle, Thierry Lefèvre, François Renaud, Anders Pape Møller, Dorothée Missé, Frédéric Thomas View Abstract
It may be seen – apart from a miserable personal experience – as an adaptive process to help either the host or the organism I think we can exclude you as the host deriving any perceived benefit, but there may be evolutionary aims here that do not make immediate sense. You may purchase the article indicated for further clarification.
Best wishes
Michael
Elvira
I was infected with B Hominis for nearly 2 years and managed to successfully eradicate it with the drug therapies from http://www.cdd.com.au/html/expertise/diseaseinfo/parasite.html
There is a wealth of info at http://www.badbugs.org
My symptoms were similiar to those of your daughter. I believe this parasite is pathogenic. It certainly was in my case as no other parasites were detected in my case other than B Hominis. In terms of diet whilst still infected, the bug seems to thrive on sugars and starches so I avoided all bread, pasta, rice, fruit etc.
Best wishes.
Tony
Hi Michael,
Firstly, please accept my apologies for the delay in replying to your very helpful comments and advice. My computer died on me and I lost all bookmarks including this one and only found your reply by doing a search on myself.
Since I wrote, I’ve been taking lots of probiotics (on an empty stomach – on advice of the GP I’ve been seeing), digestive enzymes, oil of oregano capsules and uva-ursi (both taken twice daily with food), HCI + pepsin for the low stomach acidity – all these have been prescribed by my GP. On my own initiative and following research, I have also removed all starches from my diet except vegetable starch. My diet now consists of lots of fresh vegetables and fruit, poultry, fish and occasional red meat, eggs and some dairy. In the last week or so, my symptoms have reduced considerably. I was interested in your comment about taking the probiotics with food and I would like to know why you recommend this and why there should be a few hours between taking the anti microbials and the probiotics. I should also be grateful if you would resend the link to your article on bile acids as the link above isn’t working for me. Again, thank you for taking the trouble to reply so comprehensively to my first post.
Kind regards
Rosemary
Dear Rosemary.
The probiotics are capable of being taken with or without. I suggest with as the buffering effect of the food reduces damage to the organisims, and this is the way we have historically consumed bacteria, from fermented foods or from plants or meat that has been hung. So we are equippedto handle either delivery process but mimicking normal mechanisms may confer some survival benefits.
The Antimicrobials may have a detrimental effect on the additional organisms being consumed to confer benefit. Allowing a period of a few hours gives the oregano time to move through the gut performing its intended action, then repopulating in a less hostile environment by following with organisms.
The article on bile acids is on the web site so if this does not link for you then just enter bile acids into the search box.
best wishes
Michael
Hi Rosemary
It’s years since you wrote on this topic, but I’ve just found it as I have an issue with fecal smell (think it emanates from my stomach) that I can’t smell at all and it isn’t all the time but I don’t know when or how frequently it occurs, but initially small children have said it and then I’ve had comments at work and socially from adults – its socially debilitating. I’ve just had a full stool test that shows Blastocystis hominis infection and a ‘Euryarchaeota Phylum’ that isn’t present in a healthy patient. Can I ask what treatment you took and did you stop the smell? thank you so much.
Deb
Thanks for your reply, Michael. I shall now change the timings of when I take the probiotics and the anti microbials. Kind regards, Rosemary
Is that a good idea ? Surely a meal is going to result in more acid being produced by the stomach and more likely to kill the probiotic. IMO it should be taken on an empty stomach, possible with a pinch of sodium bicarb.
Hello, a need some articles about of the relationship betwen Blastocystis sp and the Escherichia coli, because I work on my thesis, I need see the pathogenicity of the Blastocystis when is asociated to a enterobacteriaceae`s group, especially Escherichia coli.
Please Help me, with my investigation.
Hello Arturo.
Normally we encourage students to do the leg work themselves, but as it is Easter I spent a little time checking what I could. There are very few papers that describe any direct relationship, but here are a couple of quotes and refs that may assist.
Good luck – these also have full free papers
[1] Leelayoova S, Siripattanapipong S, Thathaisong U, Naaglor T, Taamasri P, Piyaraj P, Mungthin M. Drinking water: a possible source of Blastocystis spp. subtype 1 infection in schoolchildren of a rural community in central Thailand.Am J Trop Med Hyg. 2008 Sep;79(3):401-6. View Abstract
[2]Kaya S, Cetın ES, Akçam Z, Kesbıç H, Demırcı M.[Clinical symptoms in cases caused by entamoeba coli and blastocystis hominis.] Turkiye Parazitol Derg. 2005;29(4):229-231. Turkish. View Abstract
Dear Michael,
I am interested in the connection between B.hominis and H.pylori.
You mentioned that you will be reviewing B.hominis and H.pylori relationship. I could not find any article on the site..if you have done the review is it possible to send me the link?
Thank you in advance.
Petia
Hi
I have not written a review, but here are the key facts I have been able to find.
The possibility of a symbiotic relationship between H. pylori and B. hominis is quite low because H. pylori colonises the UGI tract but B. hominis, a strictly anaerobic organism, is predominantly found in the cecum.
However, H.Pylori and B.hominis havebeen found in one study to occur more frequently together. Among the 64 individuals who underwent gastric biopsy, Helicobacter pylori was found more frequently in the individuals harboring B. hominis (19 of 26 versus 15 of 38; P = 0.017).
Proposed explanation: Generally suggested that B. hominis is transmitted by the oral-fecal route, as is H. pylori. Therefore, a proportion of H. pylori may be transmitted via the same route as that of B. Hominis.
Paper for review is:
Chen TL, Chan CC, Chen HP, Fung CP, Lin CP, Chan WL, Liu CY. Clinical characteristics and endoscopic findings associated with Blastocystis hominis in healthy adults. Am J Trop Med Hyg. 2003 Aug;69(2):213-6. View Full Paper
Hello Michael
In treating b hominis, is there anything other one can do for mucosal barrier immunity than taking s.boulardii – I seem to have a bad reaction to it.
There seems to be a lot of comment on the web about how hard b hominis is to treat unless you resort to hard-to-obtain drugs – I was just wondering how effective you find the natural protocol.
Also, in your experience have you found much link between b hominis and nervous/stress/mental symptoms. There seems to be a school of thought that these things put out neurotoxins.
Thanks for your help
Peter
Hello Peter
If you have a reaction to SB, and generally only a few people do, the mannose receptors, part of your innate immune system assess it as a potential antigen and various types of responses may follow. This seems to occur where the patient may have some previous mould exposure, or a damaged mucosal barrier and or a yeast sensitivity and in more exceptional cases a yeast allergy.
The mucosal barrier will respond to other agents including just using the suggested probiotics, as well as L-glutamine, epithelial growth facor and soluble fibre. In fact grating 3 apples and eating them each day has demonstrated a significant reduction in mucosal immune activity.
Remember B. Hominis may not be the problem, you will have read that only a specific subset appear to be the problem, rather B.Hominis may simply be a reflecion of diminished mucosal immune quality and another pathogen may be the culprit- it may also have already left, leaving a residual disturbance.
Natural remedies take longer to work than medications and like medications may not be succesful. The suggested approach is to look at combining restoration with elimination and then to try medication if the symptoms and pathogen remain entrenched.
Good luck
Michael
I second this. Both are great resources for Blastocystis.
Canadian and American doctors need to WAKE UP on the problems this bug (and D. Fragilis) causes!
Things do seem to be improving but I do now need a stool test with good lab to see if Blastocystis Homonis and friends are reducing in number or gone.Can you advise.?
stella
Dear Stella
Stool tests available for commercial use look at the presence of B.hominis without a genome differentiation. This means that total B hominis count may be achieved but the virulence will not be defined. The three labs available are Genova diagnostics, Metametrix and Drs Data.
So you think testing is useful but not necessarily as authorative as we would like because the virulence of the organism cannot be defined. So it would be OK not to bother with testing but to continue to treat until improvement happens?
stella
Hi Sheila
From a patients perspective outcome is everything – from a clinicians perspective outcome and validation are sought. The subtelties in B.hominis’s genetic makeup play a predictive role in relevance of the presence of that organism to the patients symptoms. What has corrupted the overall view about B.hominis has been its presence in asymptomatic patients. I personally expect to see this develop even more as we learn how changes in our immune system lead to increase virulence susceptability from an epigenetic perspective.
Testing is useful but not as valid as outcome. If you are improving, then I suggest you continue until resolved. If the symptoms, or indeed any symptoms appear that are not transient then further investigation will be worthwhile.
Hi Micheal
Cannot continue as now getting palpitations when I take ADP….loooks like have become alllergic to the ‘cure’….don’t know what to do now? Any suggestions.
stella
Hello Stella
Just to be clear this is not a forum for one to one consultations, questions where the answer may interest other health care practitioners will be discussed, but I cannot offer a personal health care service for many reasons.
However, there are two issues in your question that merit an answer:
1. ADP is a source of time release oregano extract. You have not become ‘allergic’ to the product, this is a much overused and misused term to describe a specific range of immune responses to a selected group of provocational antigens.
2. It is also unlikely that the oregano has had any local irritation to the mucosal tissues, but not impossible. Oregano (active component cavacrol) has an anti-inflammatory effect on the gastric lining.
3. Cavacrol is a potent antimicrobial and will attack predominately gram negative organisms, but its destructive effects are not exclusive to this family of bacteria. The result is that lipoplysccharides and peroxynitrate, two by-products of microbial destruction can induce local tissue responses which includes the relase of cytokines and histamine, both messanger proteins are capable of inducing a vagal nerve response that may include alterations in heart patterns.
The more probable effect is that the rate of elimination has exceeded your mucosal tolerance and will require a repletion of suitable probiotics, prior to a reinstatement of the cavacrol. As previously mentioned, B.hominis may not be the organism of effect, and therefore the pursuit of its eradication may be unnecessary, and the collateral damage from microbial disruption may induce unwanted symptoms. The benefit of having professional support – not this site – is that an experienced practitioner can guide you through this process.
Michael
Michael: Are you saying that the mucousal barrier health is a major factor in eradicating this? And if this is restored then treatments are more effective?
As a side note I have read about the importance of beneficial e-coli as being the main probiotic of the colon, and a lab tech told me that the sickest people are those with low e coli. American research has very little to say about this but the Eastern Europeans seem to know a great deal about this. I have an article if you are interested. My levels are quite low and I am supplmenting with the only beneficial e coli product I know of, Mutaflor.
My other question is concerning the use of natural products to eradicate this. I have scoured the internet looking at studies that have been done and there is not a lot of naturals that will eradicate this. Although I am sure that not many studies have been done. Javanica Brucea, chinesis coptis, pomegranate stem and root Bark (Psidium guajaual) and Picrorhica scrophulariitlora (Hu Huang Lian) are a few I have run across. I am going to try neurolaena lobata which shows strong antiprotozoa properties but has effectiviness against other protozoa.
I have done multiple herbals including oregano oil in enteric coated caps and my observation is that they will only inhibit and not eradicate. Your comments please. Thanks.
Hi Patrick
The quality of the mucosal tissues determines the immune function and vica versa. As the mucosal tissues are the largest site for innate immune response, their ability to both neutralise, recognise and eliminate foe are a vital part of our ability to survive every day. If the immunological function in mucosal site is compromised, pathogens are harder to eradicate and commensals struggle to maintain tolerance.
Eradication success depends as much on the health of the local tissues as it does the application of an eradication strategy.
Beneficial e.coli nissele is a reconised inhabitant of the intestinal system and is unusual in the probiotic market in that it is a gram negative species, whereas as far as I am aware all others are gram positive. It has had some interesting work conducted on its clinical effectiveness and is, along with LGG recognised as a significant organism for human health. There is, as I am sure you are aware a shift from the more traditional ecological approach to the more strain specific therapeutic use of probiotics and nisselle has been one of the early strains to have some specificity attached to its mechanism of action.
The microbial balance, that is the ratio’s between the various species is as yet an unknown figure, frequency of occurance in stools of some of the principle species is a useful guide, but science is still quite way from the level of accuracy we will take for granted in a few years time.
B.hominis eradication through the use of natural agents and prescription agents is at best a challenge, and clarity of intervention is somewhat murky. This organism, as I explained can be present but also be innocent of symptom production, eradication may therefore be less relevant than bacterial colonisation and ratio changes.
The test for gene specificity is not as far as I am aware available from commercial labs as yet, so clarification of causation due to the B.hominis you have is not yet available. Suppression or management is largely how our bacterial colonies work, as a clinical view the outcome, i.e the resolution of your symptoms – whatever they are – and a return to health is more important than the elimination of B.hominis from your tests, unless they are occur mutually.
I cannot comment on the anti parasitics, I am unfamiliar with them.
Michael
Thanks Michael, these are great comments, I look forward in reading your other material.
From what I have read is that each subtype of blastocystis requires different protocols, but these protocols have not been established as far as I can tell. Metametrix tells me that they are in the process of being able to identify subtypes. I have also read that blastocystis causes so many different types of symptoms, I suspect due to the subtypes?
Hi Patrick
Sub typing as far as I can tell, has to date identified the overt gastrointestinal symptoms as being attributed to sub type 1. I suspect that other symptomatic subtypes may become identified when larger samples of infected people are analysed. However, does each subtype need a different approach, or is that each patient may need a different approach. I do not think – although I may be wrong, that the genetic variations in the species will necessarily have significant type of treatment protocols as the treatments are not gene specific, but that the gene variations of the species and the innate immune system of the infected patient may hold some valuable clues.
Obviously there are many people with B.hominis that are asymptomatic even with sub type 1 present and may remain so indefinitely, others become symptomatic after recent infection or stress and here is the subtle immune based element: Infection with another organism may so alter the microbial composition that a previously quiescent type 1 B.hominis may now be able to exert stress on the mucosa and induce symptoms, as well as the implication that a recent infection was from B.hominis and that whilst type 1 seems the most likely variant it may also be that others are inductive in the weakened tissues due to coexisting bacterial, viral or parasitic infections.
What I am trying to say is that focussing on the pathogen is only part of the story and that attributing equal importance to the mucosal immune system will provide better outcomes than trying to think of gene specific protocols.
Mike
The dialouge on this pg has been very informative!
Michael, I apppreciate the depth of your answers, and personalized attention given when responding to the questions.
Although I have done extensive internet research on B. hominis, and feel fairly well-informed, some of the info provided here is new and also greatly illuminating.
As many reading this already know, the lack of information on, or misunderstandings of this organism can be very frustrating to encounter for those looking to relieve themselves of the symptomatic form of the parasite.
And although I am recently discovering that it’s existence is much more prolific than I’d originally thought, (including in my own area of location, as it turns out,) the ignorance on the pt of medical profession, both allopathic and naturopathic, still continues to surprise me.
After struggling for years, I have decided to “bite the bullet” and opt for the combination drug therapies in hopes to completely end the battle of trying to fight this bug off. It was a very tough decision, and I can honestly say that the medications are horrible. I plan to follow up w/ natural therapies once the drug course is over- both to ensure it’s full eradication, and to also help rebuild my intestinal lining.
I am open to sharing my techniques and findings, should they prove useful to others, though much of it has been fore-mentioned here.
One area of feedback; I found this pg from an unusual word/combo search- I wish it would’ve been an easier and earlier find!
And I also have one question/theory in motion: Do you think that enzyme therapy taken at high levels, could help by consuming this parasite? I have read that the outer cell structure of blasto h. appears to be comprised of a fatty protective layer. Could possibly lipase penetrate this layer if taken systemically?
Dear LB
Thank you for your kind comments. The technical request regarding viability of enzymatic weakening of the external parasitic barrier is an interesting one. I have noticed clinically that the inclusion of proteolytic enzymes derived from pancreatic tissues confer a variety of benefits on the patient including improving the restoration of microbial balance as they appear to aid in the degradation of biofilms that in turn allows bacterial colonies to either be exposed to the antimcrobial compound or it alters their communications so that ratios may be changed – here I am speculating, but my ideas are based on published data and experience.
Lipase of course is present in the gut – so would including it has a specific effect on Bh and facilitate its eradication – I have no real idea, but it is an interesting thought and if you come up with some further mechanisms around this idea – do consider a re-post. Good luck on your own intervention -do keep inmind that whatever you are hoping to resolve may not be due to Bh anyway, but some unculturabe organism!
What about Blasto and constipation?
I have the gas, bloating, indigestion, food intolerance, psoriasis, weight loss but not the diarrhea!
Are there more people like me? Any suggestion in which direction I should look for a solution?
did have it tested, I had dientameoba fragilis with it which got eliminated by the flagyl but the blasto didn’t. Plus my whole digestion came to a stand still after the flagyl.
Could there be a connection between pancreatic insufficiency and proliferation of blastos?
I noticed that I struggle digesting fats but I bloat up terribly from carbohydrates.
What if liver en pancreas work insufficient due to partial blockages ie sediments of stones so there is not enough bile flowing to generate the digestion and motility of the intestines creating thus a favorable condition for blastos to multiply.
Could adrenal fatigue have to do with the malabsorption?
I am on sleeping tablets, I feel tired and easily stressed by everything while at the same time I am unable to get that restorative sleep by myself?
I have lost a lot of weight and I need to find a solution before I truly collapse!
Elizabeth
Dear Elizabeth
Before I provide some answers please note: I cannot make specific recommendations as you are not my patient – I can make general comments, but I suggest you find a suitably experienced practitioner to help you through this.
Your first part question concerns an apparent paradoxical component of your gut motility. You describe constipation as being present and whilst this symptom can have quite a different meaning for some people. Constipation is miserable and can drive people to distraction. You can see from the quotation below that Bh is capable of a number of GI symptoms, and whilst constipation is infrequently mentioned in a symptom list, it is a common component of Bh infection.
B. hominis in large numbers was present as the only parasite or with other commensals in 515 specimens from patients (79.6%). Of these patients, 239 (46.4%) had symptoms, the most common being:
• abdominal pain (87.9%),
• constipation (32.2%),
• diarrhoea (23.4%),
• alternating diarrhoea and constipation (14.5%),
• vomiting (12.5%), and
• fatigue (10.5%).
S M Qadri, G A al-Okaili and F al-Dayel Clinical significance of Blastocystis hominis. J Clin Microbiol. 1989 November; 27(11): 2407-2409
There are a number of strategies for resolving constipation, but as with all agents they do not work for everyone. I normally start with a buffered vitamin C powder that has a good level of magnesium in it to stimulate IL6 a cytokine that brings fluid to the gut and aids in parasite elimination and magnesium to relax the intestinal musculature plus apples – if suitable and water.
Dimentomeba Fragillis is a common bed fellow of Bh and so will present simultaneously, this is because both thrive in a situation where there is diminished mucosal immunity, either because the gut has been altered through exposure to a disturbing factor (antibiotics is the best understood) or the organisms are capable of hijacking the competence of the immune system and set up residence as an unwanted neighbour. Any protocol at elimination has the chance to further disrupt an altered GI flora ratio and provoke IBS with its various miserable symptoms. Both Bh and Df are linked with IBS.T he relative prevalence of symptoms of abdominal pain, diarrhoea, and constipation in Blastocystis infection and IBS show a remarkable similarity.
Confirmation of Infection
PCR testing of DNA extracted directly from stool specimens is considered to be the most sensitive method for the detection of Blastocystis, and represents a 10% improvement over culture. It is currently the only way to differentiate subtypes of Blastocystis, and is used in research studies where genotyping is necessary and as such is not available to clinicians as yet. As with all forms of testing PCR is also subject to corruption from poorly handled specimens and so does not represent a fail safe approach.
Bh is now the only protozoan whose presence is reported along with its quantity by US pathologists, with standardised terms such as “rare, few, moderate, and many” describing its abundance. However, several studies have found no correlation between the quantity of Bh in stool samples and symptoms, and many tests are of inadequate sensitivity to ensure all species are detected. Therefore, quantity of organisms identifiable in stool specimens may be a poor indicator of symptomatic status.
One way to improve accuracy is to include SIgA antibody profiles as this has increased accuracy of testing
Mahmoud MS, Saleh WA.Secretory and humoral antibody responses to Blastocystis hominis in symptomatic and asymptomatic human infections. J Egypt Soc Parasitol. 2003 Apr;33(1):13-30.
You ask about pancreatic enzymes and whether a deficiency would facilitate a chance for Bh to survive or proliferate, and you also mention bloating. Please see this post I wrote on bloating for more info. More likely the cause is due to small intestinal bacterial overgrowth SIBO and this condition is also linked to IBS, whilst the breath hydrogen test is still controversial there is much more confidence in it as diagnostic marker of a common complaint that further adds to GI distress. A well informed clinician will assist you with this.
It is rare for the sphincter of oddi to be involved and not have fat digestion issues as well, so whilst there may be biliary tree issues, this should be investigated by using a murphys test to start with and if positive a simple use of beet concentrates over time can facilitate a return to bile flow, and pancreatic enzyme supplementation will determine if you are symptomatically improved. The gall bladder is prone to problems – more so in women and depending on your age a good physical should be able to give you and your clinician chance to decide if further investigation is warranted.
Lastly – Adrenal fatigue. This condition is very common but difficult to fully diagnose without a good case history and I use a salivary hormone profile as well as careful listening. Lowered adrenal output of cortisol has many clinical considerations and it would be likely that it can be a co-morbid condition with your other complaints. I recommend you purchase Adrenal fatigue by Dr James Wilson, the chapters and tests will let you work this one out and the practical advice will really help – again you need to discuss your own case with a clinician involved in this field of care.
Your positive note should be that you have every chance of recovering, but will need help – good luck.
Michael
Dear Michael,
Your answer is very valuable, it brings together all the elements I had perceived but been unable to link together. My gut tells me you are right!!
This week I should get the lab results of fat in faeces and my breath hydrogen test. Which would confirm your thinking.
The insight you gave me was that my problem has not one cause but the combination of 6 elements: Blasto, chronic fatigue, constipation, bacterial overgrowth, sluggish pancreas + female hormones.
So now the treatment! I am seeing my specialist but I am interested in your opinion. Since Devon is to far away for me to come and see you (I live in the Netherlands). Would an internet consultation for nutritional
advice be possible?
If I would write my own treatment plan I would do:
1.for the BLasto you Natural strategy: Saccharomyces Boulardii, oil of oreganun, Vit A and L glutamine powder + apples.
2.For the chronic fatigue – Garum Armonica.
3.For the constipation – Vitamin C / magnesium powder.
4.For the bloating – Probiotic – LGG possible Hylak Forte.
5.For the indigestion – Pancreatic enzyme.
6.For my hormones – once I have picked up some weight! Progesterone/crème to regulate my period.
What I don’t know is in which order to take the different stuff and how deal with the digestion of carbohydrates to gain weight?
Do I miss something? Is there more I need to think about?
The very skinny Elizabeth
Hi
I have extracted the list and edited it below. I do not see patients anymore but can refer you to a colleague if so desired. Please call Nutri-Link and they will give you the details.
Here is the edited version.
If I would write my own treatment plan I would do:
1.for the BLasto you Natural strategy: Saccharomyces Boulardii, standardised oil of oregano (ADP)at 6 per day for 6- 8 weeks, Vit A 12,000iu per day 1-3gms L glutamine powder + 3 grated apples per day.
2.For the chronic fatigue – Garum Amoricum 4 per day.
3.For the constipation – Vitamin C / magnesium powder as buffered vitamin C 1-2 tspns daily.
4.For the bloating – Probiotic – LGG possible Hylak Forte.
5.For the indigestion – Pancreatic enzymes such as intenzyme forte with food.
6.For my hormones – once I have picked up some weight! Progesterone/crème to regulate my period. I do not recommend progesterone cream
These are based on general suggestions not on your personal needs – you will need to get further clarification on starting dose duration and food selection.
Mike
Dear Michael,
Thank you for your reply. I have followed your advice and contacted your colleague. I am waiting for his reply.
In the mean time I have a few more questions:
What does ADP stand for?
the apples can I grind them mechanically? Why 3? Are they used for the pectine and its liver clearing function?
What would you suggest to regulate periods? Primrose oil?
Would any of this products be of benefit to a case like mine?
pancreoflat, primaverum bromide, olive leaf extract, selenium.
Its great to find somebody with so much knowldge !
I hope that toegether with your advice and your colleages insights I can write to you in a few months time as chubby Elizabeth.
Dear Elizabeth
ADP is the trade name for a patented and standardised extract of oregano oil. Advanced Dybiotic Product. The apples are best grated using a cheese grater – the reason we ask you to gate them is the surface area is increased. I have used this technique for many years but as to why three are recommended. This was vaidated by a small study using a mouse model and a significant reduction in local inflammation was achieved with the human equivalent of 3 apples per day. I wrote about it here
The other questions are best answered by a one to one discussion with your health care professional.
Michael
Dear Michael,
This is very good work and a great contribution to this subject. You must be very busy with the enormous amount of research you’ve clearly made, Thank you.
I have read “The correct term is now Blastocystis not Blastocystis ‘hominis’ as there is no Blastocystis unique to humans.
I treated myself back in 2007 with the combo recommended by the Sydney clinic, it was Nitazoxinide, Secnidazole and Furazolidone. I since learned that Furazolidone is banned by the FDA
I took this combo therapy in March 2007, tested in Apr and May 2007, negative for BH. Tested again in Feb 2008, small amounts of BH were seen. I stayed at home and did not travel or eat out at restaurants from May 2007 to June 2008. I was very careful what I ate and could not have been re-infected that easily as doctors say, “it’s very easy to get BH”. So this famous Sydney drug combo did not work for me and the silence and reluctance of the Sydney clinic to respond to my questions confirms my doubts and makes me feel they are stabbing in the dark with using combo drugs that may do lots of harm. I still have BH, no diarreah, only bloated feeling and undigested food and flatulence.
My recent colonscopy biopsy report showed a tubular adenoma polyp was removed from the cecum and that I have light dysplasia of the epithelial of the cecum. So I am rather concerned, why so called gastroenterolgist specialists are not taking seriously the point that you mention above, namely “that B. hominis, a strictly anaerobic organism, is predominantly found in the cecum”. EXACTLY where the polyp was found, any significance I wonder?
Specialists also found via a gastroscopy, that my mucosa is steadily being destroyed and disappearing (atrophic gastritis) and the biopsy report (stomach) shows non active unspecific inflammation of the Antrum. Doctors just are waiting for this to become active before they do something: They say, nothing can be done because it is an auto immune disease (pernicious anemia & b12 deficiency) but they fail to ask why has the auto immune response (anti parietal and anti intrinsic factor antibodies) started in the first place.
Gastroenerologists are not taking seriously another point that you mentioned above, namely “type 1 B.hominis may now be able to exert stress on the mucosa and induce symptoms,” It certainly is in my case. I really wonder what these specialists are studying or doing besides earning a fortune, not much!! My only positive contribution is, people should try to avoid worry, this is stress and provokes an even worse gut reaction. When i take exercise and breath properly and avoid negative thoughts, it helps reduce symptoms. It would be interesing to hear your point of view. Thanks again, Trevor
Hi Trevor
I hope that the following helps to answer some of your questions, however, you have asked quite a few and due to time constraints I have not been able to cover them all.
I tend to focus my work on the immune system and relate this to acute and chronic infection. What can be said however is that parasitic diseases continue to cause significant morbidity and mortality throughout the world irrespective of the patient’s immune status. Various papers suggest there are approximately 340 parasite species capable of infecting humans, with the majority of the estimated 3 billion people currently infected residing in developing regions of the world.
Yet most microbiologists and immunologists will tend to agree that the risk factors for acquisition of parasitic infections are the same in both immuno-competent and immuno-suppressed individuals. So we have to ask ourselves – what is the role of the immune system in managing, resisting and eradicating parasites including B.hominis?
Our immune systems have adapted to the role of parasites over millennia and there are certain parasites that appear to confer an immunological advantage to us. We will use local and systemic responses through activation of the immune system to play an integral part in modifying the establishment of infection, controlling disease once it is established, limiting the severity and dissemination of the disease, and assisting in clearance or control of the parasite.
What this tends to mean is that immuno-suppressed patients are more likely to acquire infection after exposure, have more severe disease once the infection is established, have disseminated infection rather than localised infection, and be unable to clear parasites with chronic carriage states. The outcome of this alteration in immune competence will in severe infestations/immune suppression lead to, and account for, the greater morbidity and mortality in these patients.
However, the majority of immuno-suppressed individuals do not differ from immune competent patients in their presentation, with the major determinants of clinical severity and outcome of parasitic infection in immune suppressed patients being the degree of immune deficiency. Furthermore, with immune reconstitution through effective therapy or relevant withdrawal of immuno-suppressive agents, these patients are more likely to behave like immune competent patients.
There are currently in excess of 120 congenital immunodeficiencies either affect humoral immunity or compromise T-cell function.
Immuno-suppression may also occur in malnourished patients and this can include quite subtle variations in micronutrients, patients undergoing chemotherapy for malignancy, and those receiving immuno-suppressive therapy. However, for parasitic infections, cell-mediated (T-cell) abnormalities predominate. This means that the ability to produce thymic derived cell sets in suitable numbers to manage infection and eradication. This now includes TH17 and TH1 and TH2 T cells. Plus after a while the chronicity of infection leads to total T cell depletion – a sort of immunological fatigue. This will allow re-colonisation of the parasite in the mucosal tissues after elimination, as the testing methods cannot confirm complete elimination. Most patients will be inclined to think of a magic bullet rather than a strategic and often attritional therapy leading to disappointment when later tests identify a return.
Blastocystis spp. are enteric unicellular parasites that are the most frequently reported parasite in human faecal samples.
As you correctly note there has been a change in the naming or taxonomy of this parasite. Traditionally it was classified as a protozoan parasite, recently, due to new molecular techniques, Blastocystis has been shown to be closely related to the stramenopiles (these are a major line of eukaryotes currently containing more than 100,000 known species). However, due to it being nonmotile and not possessing flagella, in contrast to other stramenopiles, it has been placed in a new class, class: Blastocystea, in the subphylum Opalinata, infrakingdom Heterokonta, subkingdom Chromobiota, kingdom Chromista .
This as you can see results in quite a mouthful, but what it means is that Blastocystis exhibit extensive genetic diversity, currently there are at least nine subtypes (genotypes) within Blastocystis. Recent studies have shown that no group exclusive to humans exists and that all clades (a group consisting of an organism and all its descendants) have been detected in human stool. Consequently, human isolates of Blastocystis that were commonly referred to as Blastocystis hominis should be called Blastocystis spp. due to there not being a single subtype specific to humans. An altogether easier term, but one which most Labs do not use, and so I have continued to apply the older term as patients recognise this.
One of the main difficulties concerning its potential pathogenicity is that no recognised animal model exists for Blastocystis testing; this means that Koch’s postulates are unable to be fulfilled in order to confirm or exclude the pathogenic nature of this organism. This has resulted in a confused approach to consideration of validity of action and need for eradication.
You raise a question about acquisition of the organism; this is thought to occur as a result of frequent animal-human, human-human, and human-animal transmission, with reports of carriage of Blastocystis in mammals, birds, amphibians, and even insects.
However, I suspect that in your case the drug therapy was effective in reducing the faecal count to a point where you were described as being resolved, but that your SIgA and Tcell activity did not restore to the point that you could retain or regain immuno-competence and so your unwanted passenger was able to evolve to the point that it could induce symptoms and be identified in stool samples.
Atrophic gastritis (also known as Type A or Type B Gastritis more specifically) as quickly defined by Wikipedia – is a process of chronic inflammation of the stomach mucosa, leading to loss of gastric glandular cells and their eventual replacement by intestinal and fibrous tissues. As a result, the stomach’s secretion of essential substances such as hydrochloric acid, pepsin, and intrinsic factor is impaired, leading to digestive problems, vitamin B12 deficiency, and megaloblastic anaemia. It can be caused by persistent infection with Helicobacter pylori, or can be autoimmune in origin. Those with the autoimmune version of atrophic gastritis are statistically more likely to develop gastric carcinoma, Hashimoto’s thyroiditis, and achlorhydria.
Blastocystis Spp do not colonise the stomach, and I know from another post you sent me that you have had H.Pylori which may be a potential trigger, but all mucosal tissues share a common immune family and the incidence of dual infestation, atrophy and your adenoma polyp suggests that autoimmuity , genes and environmental forces are combining to influence your health.
It may be worth while seeking a clinician familiar with the functional medicine approach to gastric health care, part of which as you quickly describe is recognising the importance of stress management.
If this Blastocystis Hominis …Bacteria Parasite/Bacteria …attacks the T Cells .. .Sunlight would help the immune system to become stronger ? Yes ? Many are becoming weak ,not sleeping ,inability to concentrate also i have a sensitivity to E.M.F …before i even knew a cell Tower was anywhere near my home… I heard an electrical hissing sound,inability to concentrate …inability to sleep..when the suggercane opposite my home was cut…There was the Cell Tower in clear view …Then I knew why my HEALTH was suffering …Now i have this parasite … anyone else have these symptoms before joint pain set in ??? Thank you Michael… Lots of info here …
Dear Michael,
Ijust wonder if Entamoeba hartmanni is pathogenic? I have this parasite and I have a huge fatigue with pain over my chest and stomach as well as a lot of mucus in my stools.
Best regards,
Jamal
Hello Jamal
The genetic family of Entamoeba contains many species, six of which (Entamoeba histolytica, Entamoeba dispar, Entamoeba moshkovskii, Entamoeba polecki, Entamoeba coli, and Entamoeba hartmanni) reside in the human intestinal lumen.
Entamoeba histolytica is the only species definitely associated with pathological sequelae in humans; the others are considered nonpathogenic. Although recent studies highlight the recovery of E. dispar and E. moshkovskii from patients with gastrointestinal symptoms there is still no definitive evidence of a causal link between the presence of these two species and the symptoms of the host.
I must stress that this does not mean that the organism may not cause symptoms, but that there is no association between it being present and symptoms – this can be confusing, but the reason relates to your immune systems capability of either eliminating or accommodating its presence. To complicate matters further this may also vary on a day to day basis.
The entomoeba of concern is: Invasive amoebiasis due to E. histolytica. This is more common in developing countries. In areas of endemic infection, a variety of conditions including ignorance, poverty, overcrowding, inadequate and contaminated water supplies, and poor sanitation favour direct fecal-oral transmission of amoebas from one person to another. Being responsible for approximately 70 thousand deaths annually, amoebiasis is the fourth leading cause of death due to a protozoan infection after malaria, Chagas’ disease, and leishmaniasis and the third cause of morbidity in this organism group after malaria and trichomoniasis, according to recent World Health Organisation estimates.
There are a large number of species of amoebae which parasitise the human intestinal tract. Of these Entamoeba histolytica / dispar is the only species found to be associated with intestinal disease.
Although many people harbour this organism world wide, only about 10% develop clinically invasive disease thus the parasite has been shown to present as two very differing clinical presentations.
1. The commensal or non-invasive luminal form where the parasite causes no signs or symptoms of disease.
2. The pathogenic or invasive form where the parasite invades the intestinal mucosa and produces dysentery or amoebomas and may give rise to extra-intestinal lesions via the blood, mainly to the liver.
The pathogenic or invasive species has retained the name E. histolytica and the non-pathogenic, non-invasive species has been named E. dispar.
The indications of increased mucus can have a number of causes including parasitic infection, but also inflammation from IBD. Further examination and work with a suitably experienced practitioner is advised.
Hi Michael,
Thank you for this in depth response and your thoughts on functional medicine approach, I only just read about that this weekend and had decided to try that direction.
Incidentally, there must someone else with my name as yesterdays post was the first post I have made and I have never had H. Pylori.
Thanks again
Trevor
Hi again Michael,
I forgot to ask, you mentioned that my SIgA and Tcell activity did not restore to the point that I could retain or regain immuno-competence……
Please excuse my ignorance but is there any way to restore the SIgA and Tcell activity so that I can regain better immuno-competence, perhaps through stress control, lifestyle changes with the help of a clinician familiar with the functional medicine? I’m also bit lost so not sure how to find such a clinician.
Thank you and best regards
Trevor
Hello Trevor
SIgA is produced by the stimulation of normal bacteria and also some pathogenic or damaged bacteria in the mucous membranes. The normal clinical strategy includes the use of Saccharomyces Boulardii, lactic acid bacteria (LGG) and Bifo species (Bio Bifido BacT) plus a mixed lower order oild offering a 4:1 ration of omega 6-3.
T cell activity/balance requires different bacteria and also some herbs or immunoglobulins such as colostrum, but in all cases it can be helpful to have your immune profiling done first of all.
Functional Medicine practitioners are mainly located in the United States but there are a number in the UK and in the EU. If you call Nutri-Link on 08450 760 402 they can suggest one for you.
Best wishes
Hi Michael,
Thank you very much for your fast reply and your time.
I did 4 stool tests with fixative and the only parasite they got from me was Entamoeba hartmanni cyst and trophozoite.
I read that sometimes lab technicians cannot distinguish between the Entameba spp. Next week I will do a DNA stool test to be sure what type of parasite I have.
The first doctor I visited treated me for H.pylori. Since then my symptoms got much worst. I got jack itch and a white tongue. This make me think that I might have candida but I’m not sure. I also have a chronic burping. I burp like 100 times a day even without eating.
Can Candida cause chronic burping and stomach pain? could candida lead to parasite infection or make a non-pathogenic Entamoeba hartmanni pathogenic?
Thanks a lot again.
God bless you.
Hello Jamal
Please note – I cannot enter into personal consultations. I will answer your questions in a general way so that you may seek extra assistance.
Lab technicians are not infallible – no one is so there may have been an incorrect identification, but this is not that likely. You would be well advised to ask a different and suitable lab to do another test.
H.Pylori is normally only treated on clarification of its existence – So I suspect your first Dr did a test to look for clinical signs of its existence. Hopefully one of these:
• Siddique I, Al-Mekhaizeem K, Alateeqi N, Memon A, Hasan F.Diagnosis of Helicobacter pylori: Improving the Sensitivity of CLOtest by Increasing the Number of Gastric Antral Biopsies. 2008 Feb 13. J Clin Gastroenterol. View Abstract
• Faruqui AN, Majid U, Ahmad L, Khalil M, Hassan MU. Helicobacter pylori stool antigen test (HpSA) for the diagnosis of gastric infection. J Coll Physicians Surg Pak. 2007 Jun;17(6):316-9. View Abstract
• Rahman SH, Azam MG, Rahman MA, et al. Non-invasive diagnosis of H pylori infection: Evaluation of serological tests with and without current infection marker CIM. World J Gastroenterol. 2008 Feb 28;14(8):1231-6. View Abstract
The treatment you do not describe, but the common treatments include: metronidazole, amoxicillin, bismuth, and omeprazole (OMAB) and this combination can cause a change in the microbial balance in the gut leading to small intestinal bacterial overgrowth – a cause of burping after eating carbohydrates.
Occaisionally people aggravate the burping through the oral ingestion of air. Try breathing through your nose only when it starts to see if you bring it to a halt. Lastly increased burping may be linked to a decreased level of HCL in the stomach – this is often linked to nutrient deficiencies and stress. There is a simple test called the gastro test that clinicians may undertake to identify this. The use of HCL supplements may also be tried.
Lastly the absence or presence of candida I not related to tinea cruris (Jock itch) and fungal spores will not make a non pathogenic organism pathogenic in itself, but may mean that overall mucosal immunity is compromised so that other non-cultured bacteria can be creating symptoms.
Hi Michael,
The treatment I took for H.pylori was Hpac ( Clarythromycine, Amoxicillin and omeprazole) for 7days. From the day one I got the jack itch when I started the treatment. I felt also my ears cracking while taking the treatment.
I have to mention that after 3 day of following your recommandation about builiding the mucosal barrier and establishing the tight junction I feel like 40% better.
The remedy I’m using is fasting and taking cabbage juice with 4000UI vitamine D3 + 2 capsules of S.boulardii+ biotin+ 1 tsp of L-glutamine.
I also drink the green tea without any sugar.
What I experienced the frist day was muscule pain and also brain pain. From the second day I got more energy.
Thansk a lot Dr Ash. The mucosal barrier is really a key for health.
Thanks again.
PS: I will update fiew weeks to see how far this remedy is working.
Dr. Ash,
New to functional medicine-have a patient with newly diagnosed Rheumatoid arthritis on low dose prednisone who has no gi complaints.
GDX CDSA showed many Blastocystis. H. Pylori antigen negative. Intestinal permeability test normal.
Have you seen reactive arthritis with Bh? In general, would this be situation where one would use broad spectrum herbal support, s. boulardii, glutamine? Would you keeep testing for other possible pathogens?
Thank you.
Hi Karen
RA is a complex condition with a number of proposed mechanisms. The current strategy recommended by Rheumatologists involve aggressive intervention early on as this appears to prserve joint integrity for longer than the older progressive approach.
Bh may or may not be a problem – I am sure you will have read the previous replies. However, absence of pathogen does not mean absence of dysbiosis, as the effector organism can have long gone leaving behind commensals which because of the change to their local ecological mix are now called pathobionats – that is the immune system starts to issue inflammatory mediators against previously tolerated bacteria.
The slight increase in IP you describe can be made significantly worse on exposure to provocative foods – the most common being gluten.
Attempted eradication by whatever means – antimicrobial or antibacterial can produce outcomes of unexpected consequences – I suggest bacterial support and barrier reair and then consider a treatment plan of eradication – albeit that you will need to consider all of the relevant parts of the patients story to make your clinical choice relevant.
Dear Mum,
In NY you can find and see Dr Leo Galland who has great expertise on these matters and will be bale to assist you. I sent him a patient 2 years ago and he was of great help. The young women (similar situation to your daughter), was able to recover very well. Good luck,
Dear Doc,
Thanks for posting this. In my research, I came across your site and it is invaluable.
Meanwhile, I had a question about cysts.
Protozoa have evolved mechanisms that allow them to live under a great range of environmental conditions. When these conditions are unfavorable, most species are able to enter an inactive, or dormant, phase. They secrete a thick protective outer wall that prevents them from losing water and protects the cell from extreme temperatures. This tough little package, called a cyst, may also serve as a means of dispersal (to spread widely). Once a cyst reaches a more favorable environment, its outer wall breaks down and the cell resumes normal activity.
So the protozoa adapt to form cysts and hibernate without consuming any nutrition. So how do the cysts ‘die’ off through antibiotics or herbs? The cysts are also known to hide in ‘pockets’ of the intestines avoiding the sweeping laxatives (be it food based or commercial laxatives).
Thanks a lot for your help
Regards
Roger
Dear Michael,
I might be wrong and perhaps B.hominis has nothing to do with the mucous of the stomach but I wonder if you could clarify something for me?
I have auto immune gastric atrophy type ‘A’ and I read “B.hominis is only able to survive in a mucosally (immune) compromised host”.
With my auto immune gastric atrophy type ‘A’, am I regarded as a “mucosally (immune) compromised host”?
My recent gastroscopy showed that the mucosal lining of my stomach is worsening and I would like to try and treat my condition by fixing the mucous lining, maybe with bifidus as well as acidophilus.
Thank you and best regards
Trevor
Hi Trevor
Atrophic gastritis (also known as Type A or Type B Gastritis more specifically) is a process of chronic inflammation of the stomach mucosa, leading to loss of gastric glandular cells and their eventual replacement by intestinal and fibrous tissues. As a result, the stomach’s secretion of essential substances such as hydrochloric acid, pepsin, and intrinsic factor is impaired, leading to digestive problems, vitamin B12 deficiency, and megaloblastic anemia. It can be caused by persistent infection with Helicobacter pylori, or can be autoimmune in origin such as yours. Type A gastritis primarily affects the body/fundus of the stomach, and is more common with pernicious anaemia.
The stomach is a unique tissue compared to the small and large intestine and your condition will be linked to altered absorprtion and function. In particular you will most likely suffer from altered (diminished production of HCL) this puts you in a compromised position as down stream reactivity and mucosal health relies on the chyme that leaves your stomach being mostly acidic. Subject to confirmation that youhave low HCL production the exogenous supplementation of a suitable digestive enzyme containing HCL and pancreatic enzymes would I think offer a practical solution.
Eradication O H Pylori is also required as it is proposed that there is a linked immune reactivity to the pathogen and your gastric tissues resulting in a loss of distinguihment between you and the pathogen. This induces an increase in local immune damage but paradoxically a reduction in immune competance is linked to chronic H Pylori infection.
The H Pylori burrows into thelining of the stomach through the mucous layers and creates a microenvironment with a neutral pH. It actually survives when the area is more alkaline – so the autoimmune component of your condition that reduces HCL production places you at risk of HP infection – hence I suggest enzymes and HCL supplementation will be a better siggestion than a probiotic.
Hello Michael,
I have a few of questions I hope you have time to answer.
1) Did I understand correctly that SIgA and Tcell activity can be restored via a clinical strategy that includes the use of Saccharomyces Boulardii, lactic acid bacteria (LGG) and Bifo species (Bio Bifido BacT) plus a mixed lower order oild offering a 4:1 ration of omega 6-3? if so, can I send these notes to Nutrilink and order there?
2) You mentioned, T cell activity/balance requires different bacteria and also some herbs or immunoglobulins such as colostrum, but in all cases it can be helpful to have your immune profiling done first of all.
2a) Can I order the different bacteria and also some herbs or immunoglobulins such as colostrum from Nutrilink?
2b) Can you possible advise where I can have have immune profiling done? Would this be carried out by a Functional Medicine practitioner?
Thank you and kind regards
Trevor
Trevor
Here are my quick replies.
1. Yes I have hypothesised based on human and animal studies as well as substantive clinical experience that SIgA and respective CD25+ or induible Treg cells can be expanded in the gut and migrate to other mucous tissues via the strategy you have summarised.
2. Colostrum adds IgG and IgA in a form familiar to our gut tissues and can be undertaken without the need for extensive immune profiling as the therapy is cheap and has no risks.
3. You can call Nutri-Link and use my name, as they will not sell to individuals without a relevant practitioner referral.
4. Immune profiling can be undertaken by a number of different laboratories and many people trained in functional medicine and nutritional therapy will be familiar with this.
Hi Michael, Thank you for your answers.
Can you help with the following?
How do I confirm I have low HCL production?, and if I do not, which suitable digestive enzyme containing HCL and pancreatic enzymes could you suggest?
I have had many gastroscopies and H Pylori has never been found, neither with blood tests.
Can I order all of the following at Nutrilink?
Saccharomyces Boulardii,
lactic acid bacteria (LGG)
Bifo species (Bio Bifido BacT)
plus a mixed lower order oild offering a 4:1 ration of omega 6-3?
herbs or immunoglobulins such as colostrum.
Would you be able to please recommend a laboratory and /or qualified person trained in functional medicine and nutritional therapy.
Thank you and kind regards
Trevor
Dear Michael,
Please can you advise on the following:
What are your recommendations for a diagnosis (from Genova Diagnostics) of a B. hominis result (moderate) and presence of candida albicans (1+). I am considering your natural protocol of oregano (although I am unable to find any clinical trials for its use as an anti-parasitic). Pls can you direct me to these and also advise if oregano (ADP) can be used to eradicate candida as well? I have been advised that an anti-candida diet will assist the removal of candida, however this is rich in fibre and grains which is at odds with removal of b hominis as this parasite feeds on carbs and sugar. So there is a conflict. Pls advise and also on the order of treatment if relevant.
Many thanks for your time
Hello
I cannot respond to specific protocol questions here.
However, here is a reference for the use of oregano oil on the succesful treatment of various human based parasites including B.h.
Force M, Sparks WS, Ronzio RA. Inhibition of enteric parasites by emulsified oil of oregano in vivo. Phytother Res. 2000 May;14(3):213-4. View Abstract
This is the same oil as used in ADP.
Candia albicans is not a parasite, but a commensal, that under approprite immunological conditions may develop into a pthogen, that occupies various mucosal niches and causes differing levels of dysfunction.
Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev. 2007 Jan;20(1):133-63. View Abstract View Full Paper
You may find this article of some use also. https://www.clinicaleducation.org/resources/reviews/c-albicans-does-it-really-have-a-sweet-tooth/
Hello Michael,
It all started in March 2010 with voluminous bloody stools and diarrhea. I was treated with Cipro for 5 days and it got a little better for a very short time. I then continued losing weight and couldn’t tolerate any foods, had no energy and became depressed. Since April my diet consists of meat, small amounts of vegetables and some fruit all well cooked. Occassionally I take a multivitamin and 24 hour fermented dairy yogurt (strains L. Bulgaricus, S. Thermophilus, L. Casei). In September stool test came back positive for B. Hominis.
My health and symptons have been slowly improving since the beginning of the diet.
Is the diet starving out some of the B.Hominis. If some of the parasite is starved by diet would then the ADP emulsified oil of oregano be more successful to eridicate the parasite.
Do the following foods feed B. Hominis:
Well cooked non-starchy vegetables (consumed in medium to large quantities)
Dairy yogurt – strains – L. Bulgaricus, S. Thermophilus, L. Casei
Coconut yogurt – with the same strains
Probiotic – Lactobacillus acidophilus
Oils – Olive, Coconut, Ghee.
Animal fats
Nut flours.
Can taking the oil of oreganol drops over a long period of time with food cause irritation to the stomach. Have there been any studies or cases that the oil of oreganol alone with diet was able to eridicate this parasite.
Are tests available to determine if parasite is pathogenic.
Is this parasite easily transmitted to another human if so how? Has it been found that this spreads easily within a household.
Thank you,
Dear Giovanna
Dietary inhibition and associated improvenment in B.Hominis makes sense but there is no published data on this in humans. Essentially if the food choice favours commensals which in turn inhibit B.hominis you may expect improvements. I can see not relationship between the foods listed and risk of B.hominis increase.
Oregano also contains an active ingrediet that reduces irritation in gastric tissues called betacaryophyllin (E-BCP) and you may read more about that here: https://www.clinicaleducation.org/resources/abstracts/oregano-helps-stop-inflammation-and-bone-degeneration/
Transfer may be by human vector but there is some uncertainty albeit pets, humans and wter are recognised as likely vectors.
Eroglu F, Koltas IS. Evaluation of the transmission mode of B. hominis by using PCR method. Parasitol Res. 2010 Sep;107(4):841-5. Epub 2010 Jun 11. http://tinyurl.com/88pmfoc
Pathogenic confirmation tests have yet to make it to commercial labs and are just conducted in research labs at present.
Hi Michael,
I loved your write up. Great information for everyone.
I have a question about tenesmus. After doing a lot of research I found that tenesmus can be a symptoms of B. Homonis and D Fragilis. Ever since my trip 3 years to Dominican Republique I’ve had diarhea and stomach issue. But for the last year my main problem is tenesmus without any relief.
Thanks for your help.
Hi Pierre
tenesemus reflects a change in microbial composition and ratios – also known as dysbiosis – activation of the neural tissues by pathogens and their metabolites may result in a new set point of sensitivity leading to expulsionary actions – restoring mucosal tolerance and bacterial balance should assist in its recovery.
Hello Michael,
Thank you for taking the time to write me about Saccomyces Boulardi which I had a problem with.
I have now read all the various comments and I appreciate the time that you take for us.
I have one question about something you wrote about 3 apples. Above you said it will reduce mucosal immune activity, does this mean we should or should not eat 3 apples? According to my test, there is permeability AND almost no IgA so doesn’t this mean my mucosal immune activity is already reduced? Or am I missing some point?
Looking desperately to improve the permeability problem AND the IgA problem AND kill the Blastos too of course.
I also noticed someone’s question above where he inquired if you know anything about “nervous/stress/mental symptoms. There seems to be a school of thought that these things put out neurotoxins.” he wrote….
Could you please comment to this question if possible?
And also I am wondering if there is ANYTHING which could neutralize these proteases the Blastos make?
For example – Molybdenum (trace Mineral) neutralizes the acetyldehyde that Candida is excreting/producing into Acteyl something-else which is harmless to the body, and then gets eliminated. This has saved my life since I started taking it. Lifted a lot of fatigue and brain fog (tho the Candida has gone way down so says test results)
So I wondered if there is something similar for the excretions of Blastos.
I googled around and also found somewhere that info about Lipase possibly dissolving the fat of the B’s and plan to try it too, just haven’t found any yet isolated without some protease in the enzyme mix. Is this a different protease?
What about pancreatin and ox bile? Can this possibly help us sufferers in any way? Like to digest some of that fat the cysts are made of?
Like in that Tom Cruise Movie where the outerspace Giants ate the people….some man said in the middle of the film “They gotta have a weak spot somewhere!!!” (which they finally did…)
So I am hoping we will find out about Blastos weak spot ! SOON!
Thanks for your website.
Kind regards,
Jillene
Michael,
Thanks so much for your posts on this site – I’ve definitely found great information here I have not seen anywhere else.
I have a couple questions for you and one for Dave Hompes.
Michael:
I did a protocol of Paromycin and Idoquinol, It was unsuccessful at clearing the Blasto infection. I started taking VSL #3 to restore my flora, but got diarrhea a week after taking it.
1. I then started taking the S Boulardii and LGG, but am experiencing diarrhea on this as well. Is this normal? I haven’t started the oregano oil but will be starting that soon.
2. You recommend the ADP oregano oil at 100mg per day. The study you cited showed 600mg per day. Do you think that dosage is too high?
Dave Hompes:
You mentioned you successfully cleared your H Pylori and Blasto infection using herbal protocols and IgA/mucosal restoration. Is this the same protocol Mr. Ash is recommending or did you use something different?
I’m getting desperate to treat this and would appreciate any further advise.
Best,
TS
recently diagnosed with e.histolytica from doctor who is famous for finding this pathogen with fresh rectal smear. He is renowned for finding but many who have had his prescribed meds say it has not eradicated the infection completely. Is there a way to research the best prescription(s) for treating e.histolytica and can you say if there are any co-infections that need to be treated as well to increase successful treatment? (I have read that its possible to get rid of histolytica by treating its symbiotic bacteria)
thanks
Dear Michael,
After a stool test I heard I have Blastocystis.
My doctor says that Blastocystis often is apathogenic, but since there are no other reasons found for my abdominal/stomac pain, he prescribes Iodoquinol.
How do I know if my pain is from the Blastocystis? I have no diarrhoea. Diarrhoea is a symptom of pathogen Blast.?
Does Iodoquinol have side effects.
Reading several info on the internet in the meantime I started with a diet low in carbohydrates and sugars, so mainly vegetables and protein, but the pain is the same or maybe even more (maybe because of the proteins).
What do you advise?
Thank you very much for your help.
Jenny
Hi Michael Ash, Iam brazilian and i had blastocystis hominis. In this moment i made a treatment based on bactrim. After twenty days, my symptoms continues. I tried flagyl (five days) and anilia (four tries). How to proceed in my case? is It common? which your recommendation?
Really great information, looking forward to keeping you bookmarked and learning about up and coming therapies for treating Blasto!
Thanks
MJ.
Hello Michael. Firstly can i please just say ‘you are amazing’ I can only wish the gastroligist in my area were as knowledgable as you are. Please understand I am feeling alot better after mass amounts of herbs from my naturapath. My number 1 concern is which way to turn in eradicating this bug from my family. I have no idea how long it has been with us nor do i know who would have had it first. I have 5 children all tested positive for this bug. My first question is do u think if the parasite is in the bloodstreem it can be past on to my children through pregnancy or breastfeeding??? As im very interest if my breastmilk was infact riddled in parasites i was passing to my babies. Scince birth my daughter on my milk could pass up to 10 times a day??? Also after all ur research what exactly did you find to be the most successful remedies/ drugs at ridding this parasite. My children often pass pale green to dark green stools. Is this a problem with the liver? and on one occasion they passed white stools with black dots. Are the sandy fragments in the stool the cyst itself? As i at first though it was blood, but test came back negative to blood. My 2 year old also has bright yellow fragments in her stool. Please help me on my mission to stop this bug from reinfecting my family. Also i might just add. Do u think blasto can be passed dowm from generation to generation? As my of my forefathers ebded up with different intestinal cancers. Please give me advise at where to turn on eradicating eg exact drugs that have infact proven success. Thank you in advance. I am so looking forwarsd to ur reply
I also feel like there is a large link between mold exposure and blasto h. Reason for my thoughts are my 5 children could not have all digested feices specs at some point, we are very hieginic. I think a question that should be asked with all ppl that carry the bug is if they have been exposed to mold. . . I just have a strong feeling as we brought this house there was mass amounts of mould that we had cleaned. Either the damp in the air or the mold itself plays apart in this organism. Also ppl that are beeing treated should eliminate the mold to prevent reinfestation, as believe we can rid it, we just need to also rid what could possibly causing this.
Hello Jennifer
B.hominis and moulds share different taxonomy, that is they are not interchangeable organisms. However, the ability to respond in a succesful and non exogenous manner depends on the co-ordinated efforts of multiple immune responses, some of which may be compromised if already dealing with a difficult to eradictae pathogen such as some types of mould. There is extensive research on mould by Dr Shoemaker http://www.survivingmold.com/ that you may find interesting and helpful. Hygiene is of course important to avoid transfer of B.hominis, but it may be that the original infection occured from outside contact of your family – not everyone manages to obtain the same level of hygeine protection that you may do.
Hello Michael,
In your previous comments i noticed you suggest taking 6 tablets of ADP/day (im assuming this would be 2 tablets 3 times a day with a meal). I want to know why you suggest only 6? That comes out to be only 100mg/meal (300mg daily) whereas in a study i read they used 200mg/meal (600mg daily) to eliminate B. hominis. Here is the study: http://dsdinternational.com/PDFs/OilofOreganostudy.pdf .
Thank you for your time,
-Yuliya S.
Hello Yuliya
Thank you for your comments and your observation of the dose differential. My experience has been that 300mg per day is effective as a treatment dose in most patients, however, up to 600mg may be used where the product is standardised as discussed in the paper. I also suggest additional interventions so that the effect is one of synergy rather than one driven by MIC requirements. It is less difficult for the patients as higher doses can be difficult to manage and also facilitates a co-ordinated management of the innate and adaptive immune responses in the gastro-intestinal tract.
Best wishes
Michael
What do you think of the advice of rotating natural supplements? Is it true that Blastocystis becomes resistant to a treatment if continued for more than five days?
Hi Simon
There can be benefits for the host to have periodic alterations in exposure to bth natural and pharmacological agents as some resistance may ultimately develop. However, in terms of 5 days, here I suspect there is a bit of guessing taking place, as in order for an organism to be adequately exposed to a mutating compound and then alter its genome adequately to be able to resist subsequent exposure is to some degree an unknown, but I would suggestthat it would take a lot longer than 5 days.
Thank you so much for your reply. It makes a lot of sense. Also, if you don’t mind, may I ask you how often you would re-test?
Retesting is to an extent driven by symptom management. Typically at least 3 months after the treatment has begun I would suggest a re-evaluation, the results should not be viewed in isolation, but as part of the overall assessment.
Hi Michael. I recently discovered I had B. Himinis. Went through treatment which included nitazoxanide, metronidaoke, and iodoquinol. Now after a few months, a stool result confirmed the presence of the parasite again. What are my options now?
Hi Michael,
Thank you so much for your article. It is so easy to feel alone with this parasite as it seems so little is known about the effects that B. Hominis has on it’s host. I wanted to ask you about one of your replies where you said that B. Hominis can only survive in an immune compromised host. Are you referring to the individual. I was diagnosed with having the parasite B. Hominis over a year ago now, and after a series of antibiotics upon retesting I was informed that the medicine had managed to eradicate the parasite (although I do not recall being given Metronizadole). My concern with your statement about the immune compromised host is that I have been tested for HIV and it has been negative, I have also been tested for auto-immune diseases and they have all been negative. A year later, I am still having similar symptoms, I have been diagnosed with parasitic initiated IBS after a thorough exam and colonoscopy and endoscopy. Why are you saying that one must have an immune compromised system, this is the first I have heard of that. I would also note that I have within the past 6 months been having joint pain associated with the typical abdominal pain, diarrhea, fatigue, flatulence. Thank you again for your article.
Billy Crocker
Hello Billy
Many thanks for your question. You ask a good one, I hope to be able to explain some of the relevance to you in my short answer below.
BH and other parasites are able to manipulate the immune system to resist expulsion, they do this through a complex mix of genes, enzymes and other signalling chemicals. In a human with reduced immune competence – which may range from a systemic chronic infection to a loss of mucosal IgA the adhesion and resistance of the organism has been shown to be more resilient, that is it resists eradication strategies, and will persist.
One of the eventual consequences of eradication may be a ‘reprogramming’ of key immune markers and receptors as well as the bacterial ratios in the mucosal tissues, that leads to hypersensitivity of receptors and may be expressed as IBS.
Irritable bowel syndrome (IBS) is a common gastrointestinal disorder characterised by abdominal discomfort and altered bowel habit with no abnormality on routine diagnostic tests. In some patients, IBS symptoms arise de novo following an exposure to acute gastroenteritis (GE). This phenomenon, known as post-infectious IBS (PI-IBS), denotes the persistence of abdominal discomfort, bloating and diarrhea that continue despite clearance of the inciting pathogen. A systematic review and meta-analysis demonstrated that the risk of developing IBS increases six-fold after gastrointestinal infection and remains elevated for at least 2-3 years post-infection.
• Thabane M, Kottachchi DT, Marshall JK. Systematic review and meta-analysis: The incidence and prognosis of post-infectious irritable bowel syndrome. Aliment Pharmacol Ther. 2007;26:535–544. http://tinyurl.com/b8ydj9e
The current conceptual framework regarding the pathophysiologic mechanism for PI-BS suggests that PI-IBS is associated with altered motility, increased intestinal permeability, increased numbers of enterochromaffin cells and persistent intestinal inflammation, characterised by increased numbers of T-lymphocytes and mast cells, and increased expression of proinflammatory cytokines. This therefore suggests that an exposure to pathogenic organisms disrupts intestinal barrier function, alters neuromuscular function and triggers chronic inflammation which sustain IBS symptoms.
best wishes
Michael
Hi Michel
I have been found the following parasites.
– B Horminis
– Dientamoeba Fragilis trophy
And also No Yeast or few yeast but IgA is only 60.80
But my doctor suggested to take the following drugs but are they antibiotic
– Paramicrocidin250
– A.D.P
– Perm A Vite
Hello Ibrahimii
Thank you for you question.
The products mentioned are all food supplements, not medications; whilst they have the capability of treating the infectious organisms mentioned, they may not prove strong enough and a joint medication and supplement protocol may need to be implemented.
You will need to use them and see if they help symptoms and objective markers improve.
Best wishes
Michael
Hi Michael
Thank you for his very useful article and your diligent responses to everyone’s posts.
What are your thoughts on parasite induced lactose intolerance?
And secondly, can you recommend any practitioners in London familiar with Blastocystis and who can advise on ‘healing of the gut’ and improving immune system through gut health generally, including methods above?
Many thanks
Derrick
Hi Derrick
Thank you for your kind comments.
Parasite induced lactose intolerance is a manifestation of altered enzyme secretion driven by the presence of a parasite in the GI tract. The impact on lactase enzymes will naturally vary between parasite and human involved.
The brush border (BB) lining the surface of the small intestinal epithelium provides the major interface for nutrient absorption. Reduction in the surface area of the microvilli is linked with impaired levels of disaccharidase enzymes such as sucrase and lactase that are essential for proper digestion and absorption of sugars.
Several infectious agents, such as rotavirus and human immunodeficiency virus as well as non-infectious causes including coeliac disease, iron deficiency and vitamin A deficiency are reported to be linked with decreased intestinal disaccharidase activity. Reduced BB surface area has been documented in human and murine giardiasis. Reduced disaccharidase activity has been previously reported in murine, humans and gerbil models of infection with Giardia muris and G. duodenalis infected gerbils exhibited symptomatic disease, and reduced BB enzymes were evident from day 10 post-infection and onwards.
There are a number of Nutritional Therapists familiar with the treatments described above, you may find them through the British Association of Nutritional Therapists. My colleague Antony Haynes is also experienced in this treatment approach and he is based in London. You may e mail him here: [email protected]